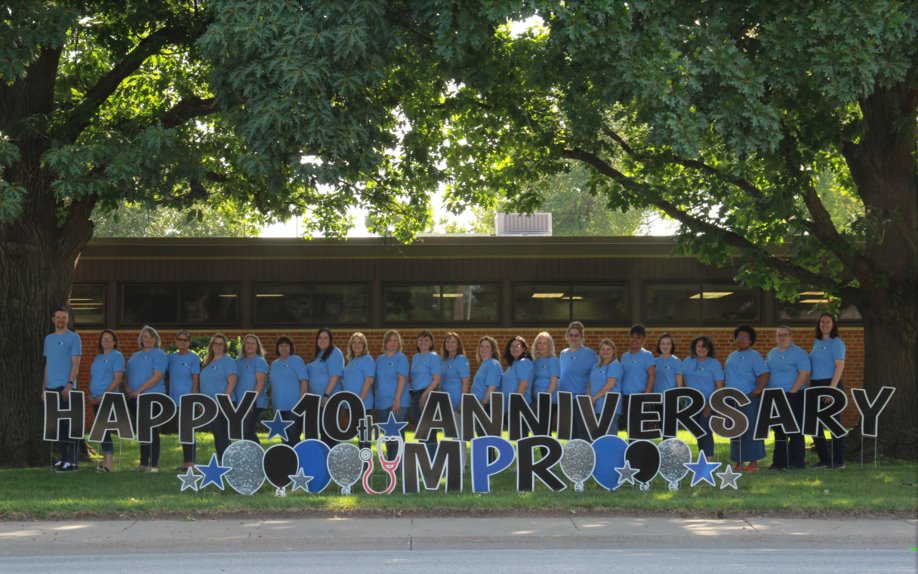
TRUSTED CREDENTIALING AND ENROLLMENT SERVICES
Let our experts handle the complicated, time-consuming burden for you.


PROVIDER ENROLLMENT
Medical Provider Resources takes the hassle out of enrolling in the myriad of insurance plans & programs. From Medicaid & Medicare to NPI & CAQH – we serve Kansas, Oklahoma, Missouri, Colorado, and Nebraska for insurance enrollment. Let us handle the paperwork processing nightmare for you!
WHAT OUR CLIENTS SAY
Love MPR! Each person at MPR is tremendously helpful! Having a one-stop shop for my initial appointments and reappointments and document updates really makes my job as medical staff coordinator easier and streamlined.
In addition, having a real person on the other end of the email or phone to help with credentialing questions is very useful and a wonderful resource in my work! Thank you for being such amazing and reliable experts. Wonderful experience to work with.
I love working with MPR. Everyone is very friendly, helpful, and efficent. You are always quick to respond when I have questions. I would never consider using anyone but MPR!!!
MPR handles our insurance enrollments professionally and efficiently. Each specialist has years of experience working with the different insurance companies. This frees up precious time and allows me to focus more on my job.
WHO WE WORK WITH
OUR PARTNERSHIPS


Medical Provider Resources is proudly local and a member of:
- Greater Wichita Chamber of Commerce
- Kansas Medical Group Manager’s Association
- Missouri Medical Group Manager’s Association
- Associate Member of Kansas Hospital Association